Reputable scientists like Dr. Michael Gershon, dubbed the father of neurogastroenterology, believe that humans have a second brain in the gut.
With the brain and the gut working in a bi-direction, they could affect each other's functions and significantly impact anxiety, cognition, depression and stress, as shown in the study published in the journal Nutrition Reviews.
This explains why antibiotics that disturb the gut microbial ecosystem can cause neuropsychiatric effects, interact with psychotropic medications and/or influence our mood, according to a study published in the Harvard Review of Psychiatry.
This also explains why mood disorders are so prevalent in patients with irritable bowel syndrome, as indicated in the study published in Gastroenterology.
Association between neurotransmitters and the gut microbiome
Chemicals implicated in depression and happiness, such as serotonin, are also found in the gut.
Research in Scientific Reports has shown that more than 90 percent of serotonin is synthesized by the gut. Serotonin is a neurotransmitter that controls your mood and is responsible for happiness, optimism and satisfaction.
Most modern-day antidepressant drugs, known as serotonin reuptake inhibitors (SSRIs), act by increasing the amount of serotonin available to brain cells.
Scientists have found that gut bacteria produce many other neurotransmitters, such as acetylcholine, dopamine, gamma-aminobutyric acid (GABA) and norepinephrine, which are critical for anxiety, concentration, mood, motivation and reward.
The gut microbiome can cause changes in how brains react
A UCLA study published in Gastroenterology investigated whether the consumption of a fermented milk product with probiotics twice daily for four weeks by healthy women (with no gastrointestinal or psychiatric symptoms) altered brain intrinsic connectivity or response to emotional attention tasks.
Researchers reported that there were significant differences in how the brains reacted during the emotional task. The group of women who consumed fermented milk for four weeks had calmer brains during the emotional task. The no-intervention (no yogurt) group showed the opposite trend – more brain hyperactivity during the emotional task.
Exposure and consumption of good bacteria are necessary for a balanced brain
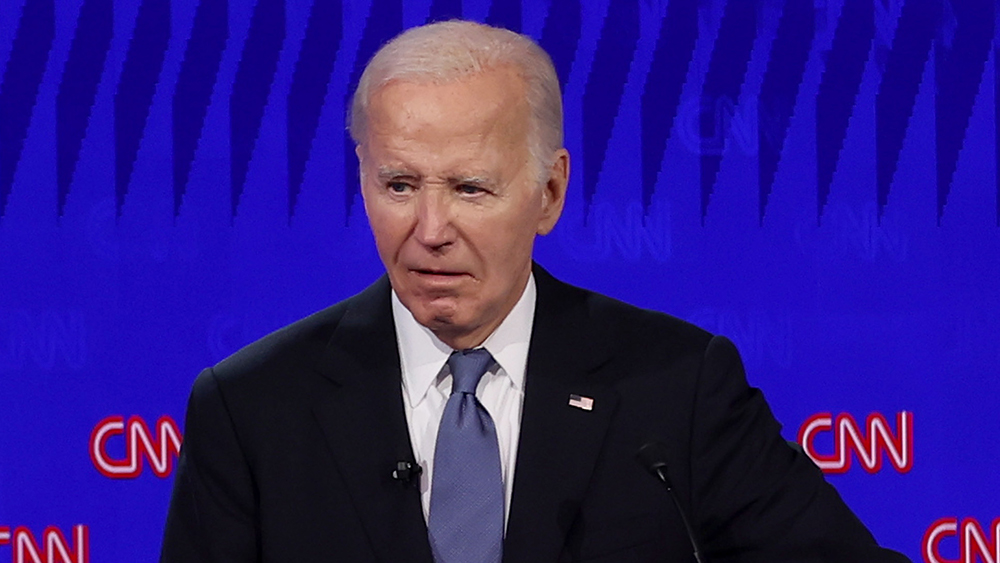
There are significantly more pro-inflammatory cytokines in depressed people compared to non-depressed ones. This effect on the inflammatory system may stem from interactions with a dysfunctional gut microbiome in depressed individuals.
Stress makes you more likely to develop mood disorders and makes the gut more permeable to bacteria. Reciprocally, depression causes dysbiosis – an imbalance of good to bad gut bacteria. In sum, depression may be caused by dysfunctional gut-brain-immune system interactions.
Good gut bacteria or the absence of some bad ones can make people more resilient to depressive states after stressors or trauma. (Related: Promote gut health with these 4 powerful spices.)
It is not surprising that chronic exposure to stress is associated with a higher incidence of anxiety, depression and post-traumatic stress disorder (PTSD). But not everyone who faces stress develops a mood disorder and not everyone who experiences a trauma develops PTSD, according to Dr. Marwa Azab, an adjunct professor of psychology and human development at California State University, Long Beach.
In a large population study (part of the Flemish Gut Flora project) published in Nature Microbiology, not only did the researchers find a link between the gut microbiome and mental health but they were also able to catalog the exact names of bacteria associated with depression and good and bad quality of life.
Butyrate-producing Faecalibacterium and Coprococcus bacteria were consistently associated with higher quality of life indicators. Dialister and Coprococcus species were also depleted in depression – even after correcting for the confounding effects of antidepressants.
What has become evident is that patients with psychiatric disorders have different populations of gut microbes compared to microbes in healthy individuals. Also, stress and stress hormones like cortisol can have a negative impact on the microbiome. All of these factors interact in complex ways with the immune system, said Azab.
Take care of your gut bacteria for good quality of life, better mental health and a sharper brain.
Visit Digestion.news for more articles about gut bacteria.
Watch this video to learn how gut health is directly connected to your immune health.
This video is from the Thrivetime Show channel on Brighteon.com.
More related stories:
A healthy gut is a healthy body – but how does it work?
Gut microbiome found to be permanently distorted by H. pylori bacteria.
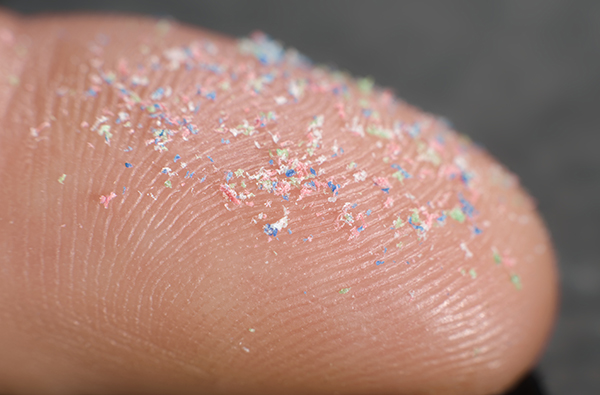
Roundup (glyphosate) found to cause alarming changes in the gut microbiome.
Sources include:
Please contact us for more information.