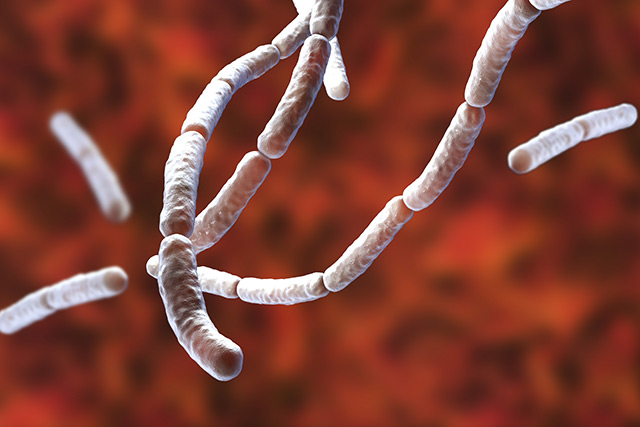
Antibiotics weaken innate anti-viral immune response in lung cells
Researchers from Francis Crick Institute, a biomedical research centre in London, learned that antibiotics weaken first line immune response in the lungs by altering the microbiome. The damage was observed in the immune system of rodents after a two week course of antibiotics. The antibiotics weakened a first line of defense in the lungs called type I interferon (IFN?/?). This immune suppression made the rodents more susceptible to influenza and made it harder for their immune system to fight the virus post infection, leading to more severe symptoms and complications from the flu.
Primary care physicians have been carelessly prescribing antibiotics for decades, putting patients at increased risk of influenza infections, while instigating complications from the flu. Antibiotics are not only speeding up the evolution of pathogens but they are also destroying innate immune response to viruses, allowing common infections to become more severe and deadly. About 700,000 people die yearly due to drug resistant infections that are taking advantage of weakened immune systems.
Rodents, not exposed to antibiotics, “over produced” these innate immune signals and were less likely to catch the flu at all. When a virus breaches the immune system, the body will send out IFN?/? signals, triggering a form of inflammation that selectively targets the virus without damaging healthy tissue.
“This study supports that taking antibiotics inappropriately not only promotes antibiotic resistance and wipes out the commensals in your gut that are useful and protective, but it may also render you more susceptible to viral infections,” concluded Dr Andreas Wack, leader of the study.
Furthermore, the researchers were able to reverse immune suppression by transplanting fecal matter from the healthy mice to the weak mice that were damaged by antibiotics.
Anyone who takes antibiotics is immuno-compromised, more susceptible to viral infection, and at risk to complications from influenza
The rodents with a productive IFN?/? response were more resistant to the flu virus from the onset. If an infection did take hold, the viral load was significantly reduced after eight hours. After two days, the virus did not take hold and a subsequent immune response never fully kicked in because it was not necessary. These rodents recovered more quickly and didn’t suffer from complications. When these same mice were given antibiotics for two to four weeks, the innate anti-viral signals they once possessed began to diminish.
The antibiotics decimated the innate signaling in the rodents’ lung stromal cells, the connective tissue that encases the lungs. The researchers could only restore this innate immune response by transplanting fecal matter of healthy rodents to the immune-suppressed ones. The fecal transplant boosted the population and diversity of gut bacteria, helping these living commensal bacteria species mediate innate immune response in the lung cells again.
“This and previous studies demonstrate that microbiota-driven signals can act at multiple levels,” said Dr Wack. “[The signals] induce an antiviral state to control infection early on, enhancing the functionality of immune cells later in infection.”
"Previous research has suggested that the microbiota-driven signal in lung stromal cells could originate either from the gut or the lung," Wack says. "However, in the work presented here, the results of the fecal transplant experiments strongly suggest a gut involvement in this effect. We would love to understand the exact nature of the signal from the gut to the lung, and we are working on several hypotheses."
Learn more about the importance of gut health and the risks of antibiotic use at Superbugs.news.
Sources include:
Please contact us for more information.