The researchers were investigating chromosome 6, one of the 23 pairs of DNA molecules found in humans. This particular chromosome contained around six percent of the total genetic material in a cell, including more than 100 genes connected to the human immune system.
University of British Columbia, Okanagan (UBC Okanagan) researcher Christina Haston reported that chromosome 6 was somehow connected to the risk of radiation-induced pulmonary fibrosis. Certain genetic material in the chromosome appeared to dictate whether or not the lung would sustain additional injuries after undergoing radiation therapy for lung cancer.
"Currently, 50 per cent of cancer patients in Canada receive radiation therapy as part of their treatment course," Haston said. "In addition to effects on the tumour, up to 30 per cent of these patients develop side effects to this treatment, or injuries to non-tumour tissue." (Related: This African shrub shows remarkable anticancer potential.)
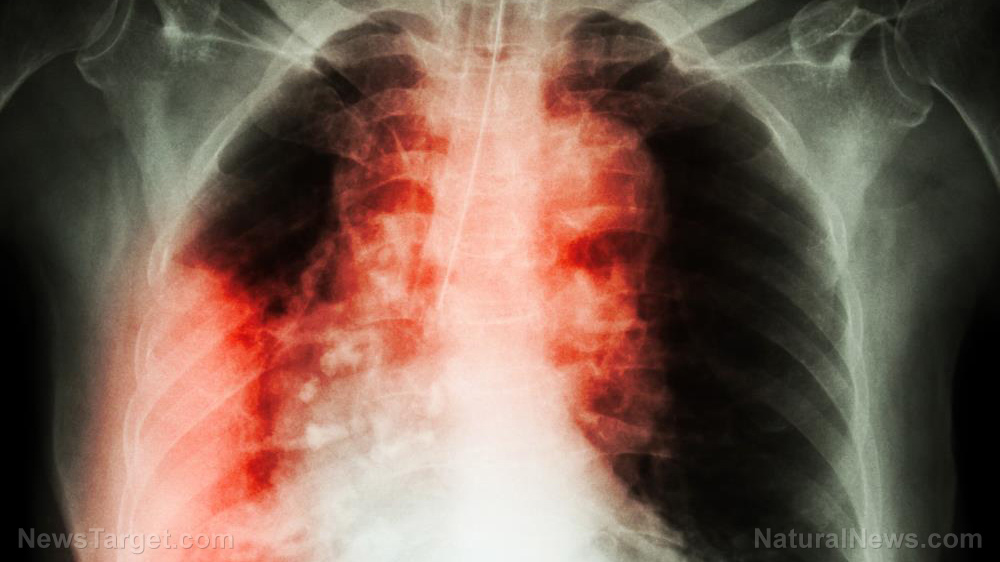
Your lungs could get scarred after getting irradiated or treated with chemicals
Pulmonary fibrosis is a progressive disease caused by the scarring of injured lung tissue. The scar tissue that developed on the organ is thicker and stiffer than healthy tissue.
Fibrosis hampers the normal expansion and contraction of the lung. This reduces the amount of oxygen that could be drawn with each breath, which in turn decreases the amount of oxygen available for use by the body.
There are lung cancer patients who experience pulmonary fibrosis after getting exposed to radiation, such as during thoracic radiotherapy treatment. Other patients suffering from different types of cancer develop this lung condition after taking Bleomycin (Blenoxane), a pharmaceutical drug used for chemotherapy.
"One of the limiting side effects of thoracic radiotherapy is the development of pulmonary fibrosis in a susceptible subpopulation of treated patients," Haston remarked. "However, the specific pathways contributing to fibrosis susceptibility in radiotherapy patients remain unidentified."
Previous studies have suggested that pulmonary fibrosis is in part attributed to white blood cells. One of the natural defenses of the body, these immune cells move throughout the body in search of pathogens.
Some of the genes in chromosome 6 oversaw immune responses, including white blood cells. Haston came to believe there was a connection between the chromosome and the risk of fibrosis.
Study says radiation and chemotherapy trigger certain genes linked to pulmonary fibrosis
Under her guidance, the UBC Okanagan researchers created two animal models using mice. One model simulated radiation therapy for cancer patients, while the other one replicated chemotherapy treatment using Bleomycin.
Some of the mice were deliberately bred to lack white blood cells. Others were consomic animals; their chromosome 6 came from another strain of mice that did not have a compromised immune system like their parent breed.
Haston reported that the mice whose chromosome 6 came from a healthy strain did not develop pulmonary fibrosis, even after getting irradiated or dosed with the chemotherapy drug Bleomycin. She interpreted these results as proof that chromosome 6 contained the genes that governed the risk of lung injury related to either radiation or strong chemicals.
Based on the results, she recommended that the genetic makeup of a cancer patient must be examined in order to determine the safest treatment for their disease. If a patient displayed the specific genes that indicated their greater vulnerability to pulmonary fibrosis, they should avoid radiation therapy and chemotherapy in order to prevent pulmonary fibrosis and other serious side effects.
Haston published her team's scientific paper in the journal Radiation Research.
Sources include:
Please contact us for more information.