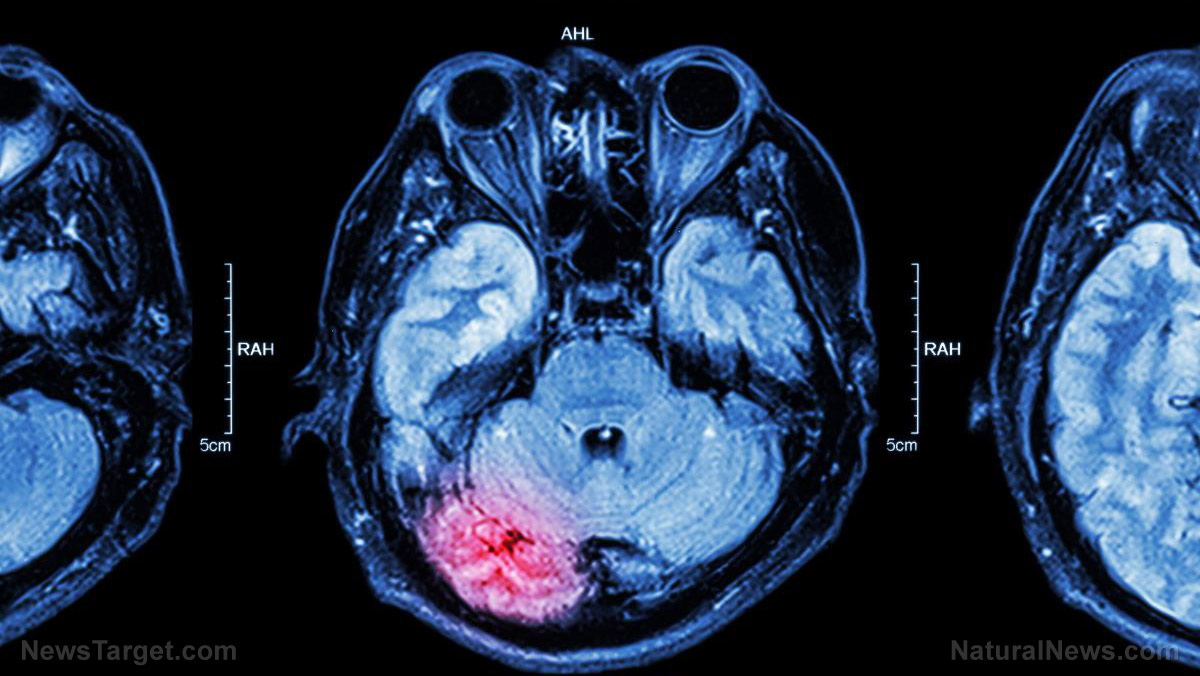
Cooling the brain was previously believed to decrease the harmful inflammation and biochemical cascades caused by traumatic brain injury. This would preserve more of the brain functions of the patient over the long term.
However, studies conducted to determine the actual effectiveness of brain cooling contradicted each other. Some claimed it was effective at improving neurological outcomes while others reported a disappointing lack of effect.
Researchers from Monash University (Monash) conducted a massive randomized clinical trial that involved more than 500 patients with traumatic brain injuries. They reported that only 48.8 percent of the participants who underwent brain cooling displayed better brain functions six months after treatment.
In comparison, patients who had normal temperatures during treatment experienced slightly better results at 49.1 percent. (Related: Delicious remedy: Licorice is a potential treatment for ischemia-induced brain damage.)
POLAR study determines whether or not brain cooling works
The Prophylactic Hypothermia Trial to Lessen Traumatic Brain Injury (POLAR) trial was conducted in six different countries. Most of the patients were men and around 70.6 percent were diagnosed with diffuse brain injuries.
The Monash-led research team divided the participants into two groups. The members of the hypothermic group received brain cooling as early as possible, either while they were being transported to the hospital or in the emergency department. Meanwhile, the normothermic group was treated in normal temperatures.
To induce hypothermia in the hypothermic group, the researchers applied cold intravenous fluids and wraps that cooled the surface of the body. They sought to maintain cold temperatures of 91.4 F for patients who were not at risk of bleeding.
Hypothermic participants who might be bleeding were cooled to 95 F. Normothermic patients were kept at warmer temperatures of 98.6 F.
The temperature management for both groups lasted for seven days. Patients treated with brain cooling were gradually warmed up after the seventh day.
"POLAR is the largest randomized trial done on this topic and the findings are very clear: cooling the brain as early as possible after head injury does not improve long-term patient outcomes and has important complications," stated Monash researcher and study leader James Cooper.
Putting traumatic brain injury patients in hypothermia does not help them, says study
The results of Cooper's study showed that the brain cooling group just barely lost out to the normothermic group when it came to the number of positive outcomes resulting from the treatment. Furthermore, both groups displayed more or less similar secondary outcomes, which included mortality rates for hospital discharge periods and six months after the treatment.
The hypothermia group also displayed higher changes of suffering from adverse events. Participants who received brain cooling turned out to be more vulnerable to intercranial bleeding, intensified bleeding, and pneumonia.
The Monash researchers noted the difficulty in maintaining the brain cooling protocol during the experiment. One out of every three hypothermic participants only got 48 hours of brain cooling, and 24 percent of them never experienced the desired temperature.
The researchers partially compensated for this problem by disregarding intracranial pressure when it came to selecting participants. They also noted that this problem was part of real life.
"Yet, this may reflect the realities of utilizing prophylactic hypothermia for patients with severe TBI in clinical practice, and there was still no benefit noted in the per-protocol or as-treated analyses," Cooper wrote in the scientific paper detailing his team's findings.
Find out more ways to protect and improve the health of your your brain at Brain.news.
Sources include:
Please contact us for more information.