Patients who take antibiotics already have weakened immune systems and depleted microbiome terrains, so they are at a greater risk to these super bug infections. Health authorities don't like to admit this and may divert the real cause of a patient’s death. Super bug outbreaks can be easily “swept under the rug” so the public is not alarmed, but the truth is staring at us in the face.
Whistleblower comes forward at hospital in Limerick, Ireland
A whistle blower has come forth at the University Hospital in Limerick and has linked 29 patient deaths to a quiet multidrug-resistant superbug outbreak at the hospital. The whistle blower called out the ongoing failure of hospital health managers who have failed to address the problem and control the outbreak, which dates back to 2009. She has called for an external, independent investigation into the deaths and the ignored outbreak that was at its worst from 2012 to 2014.
When the whistle blower alerted the Health Information and Quality Authority in 2014 about her concerns for failing infection control methods, she was ignored and even targeted by some of her colleagues. However, when inspectors arrived at the hospital, they published a report criticizing the hospital’s failing efforts to limit the spread of infection.
As national infection control teams dispatched to the hospital, new cases of multi-drug resistant infection continued to surface. In the second quarter of 2016, eight cases were detected. Three more cases linked to the hospital cropped up at a local nursing home.
The whistle blower also went to the Minster for Health. She sent him a protected disclosure listing the 29 deceased patients who tested positive for multidrug resistant bacteria and whose deaths were “associated” with hospital management negligence. Minster for Health Simon Harris reached out to the hospital and asked if the staff was properly “managing healthcare-associated infections and anti-microbial resistance in line with national standards, in order to minimise risk to patients.”
A 2011 letter, written by the hospital’s own infection control team, expressed concerns to management about hygiene, cleaning, and antibiotic prescribing practices. Another letter reveals that staff managers had grown complacent to the problem of super bug infections. One manager said that a super bug called KPC had become endemic in the hospital.
These silent super bug outbreaks continue on because authorities won’t disclose the ongoing problems of antibiotic resistance. Health authorities at Tallaght Hospital in Dublin refuse to disclose the severity of an outbreak of drug resistant carbapenemase-producing Enterobacteriaceae (CPE).
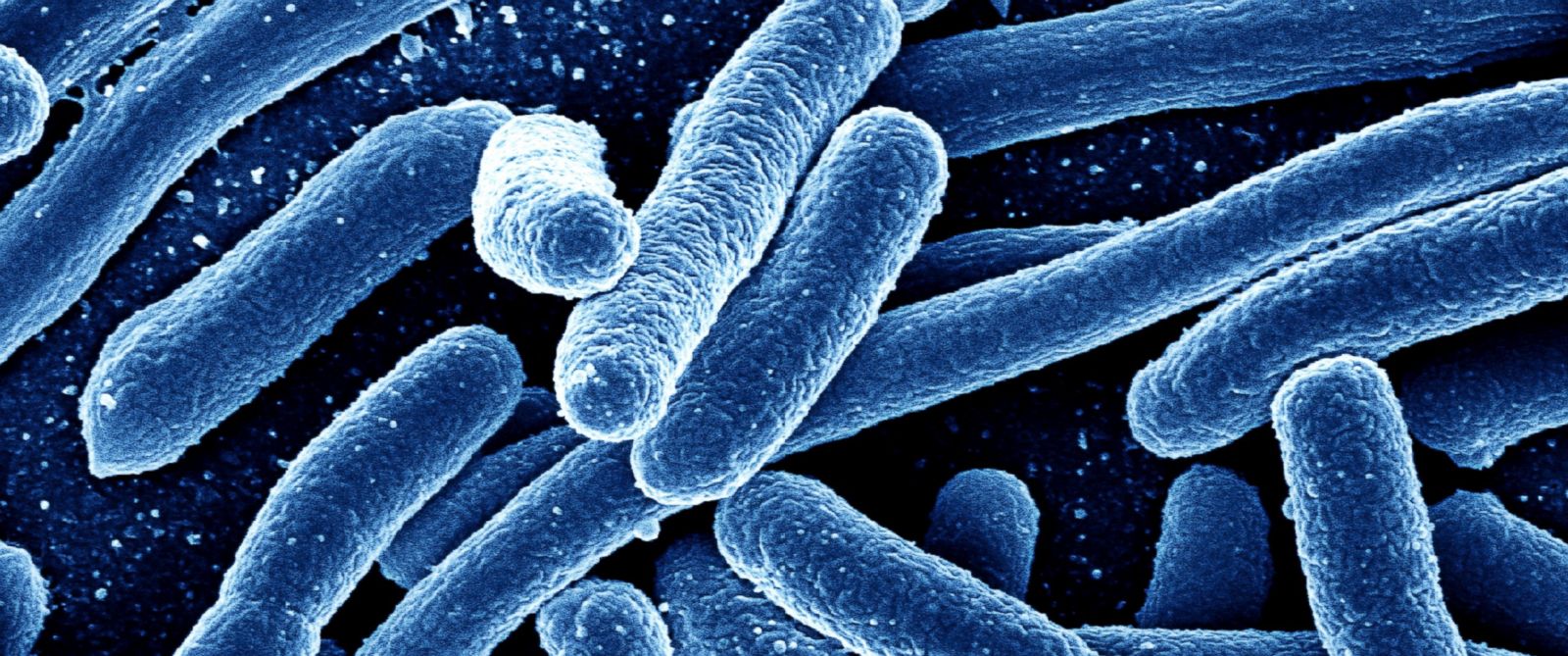
Projection: 10 million deaths per year due to antibiotic resistance
The disastrous situation of super bugs is only projected to get worse. CDC data shows that at least 50,000 deaths have now been caused by antibiotic resistance in the US and Europe alone. The global toll of antibiotic resistance is projected to reach 10 million deaths per year by 2050. It will be a greater problem than the cancer epidemic, which has taken the world by storm in recent decades. These projections are based on a large multi-faceted review project called the Review on Antimicrobial Resistance, commissioned by UK Prime Minster David Cameron a little over a year ago. The project warns about the ongoing evolution of drug resistant HIV, TB and malaria as well as drug resistant MRSA, E. coli and Klebsiella pneumonia.
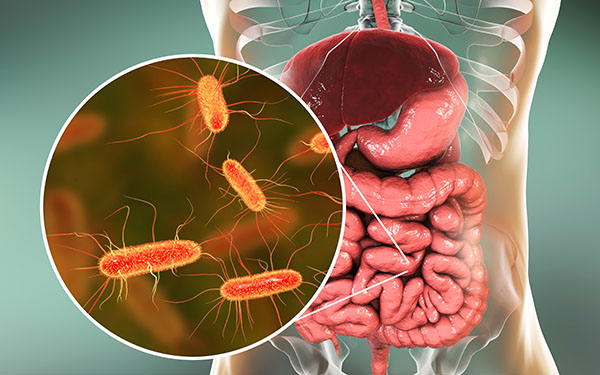
The only way to restore balance to the world of bacteria is to encourage the emergence of commensal microbes. We must investigate what it will take to re-establish the commensal microbiota of our hospital environments, and we must learn how to strengthen and diversify the probiotic species of our microbiomes in and outside our bodies.
Sources:
Please contact us for more information.