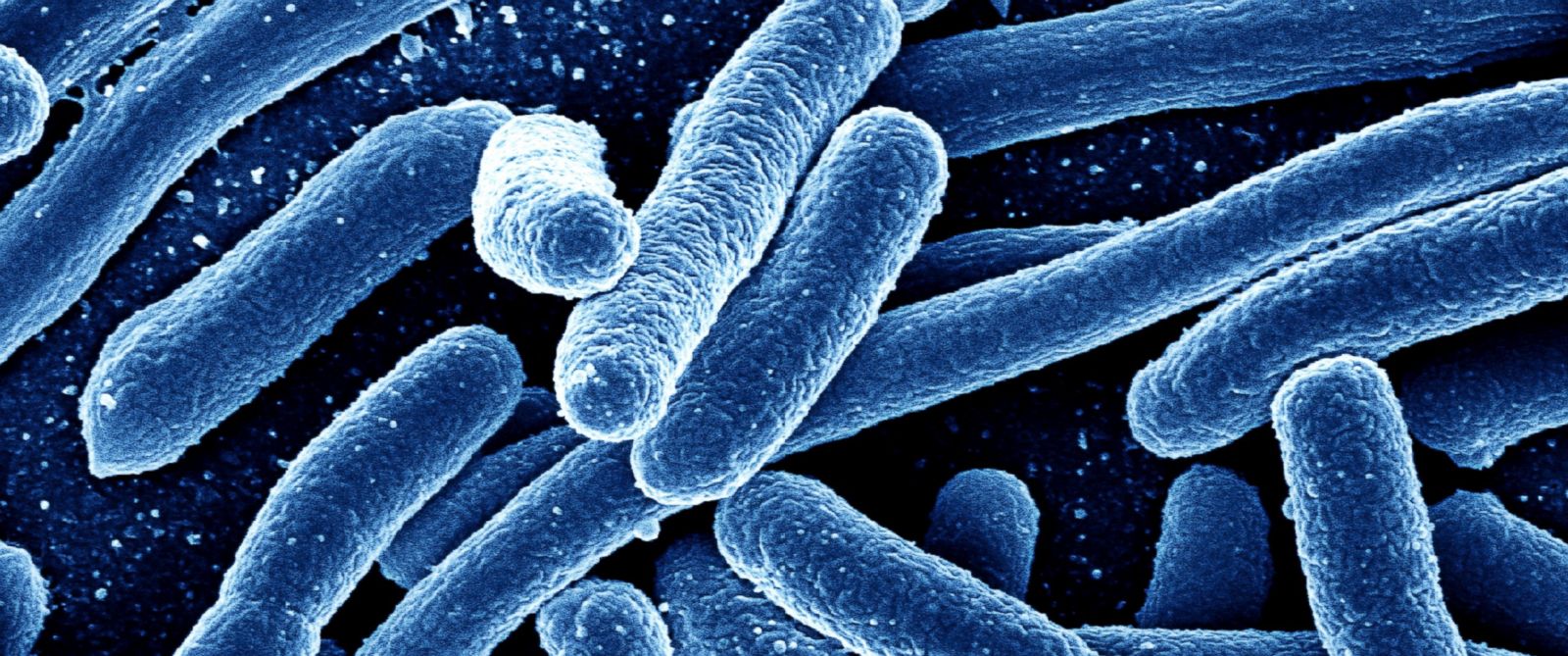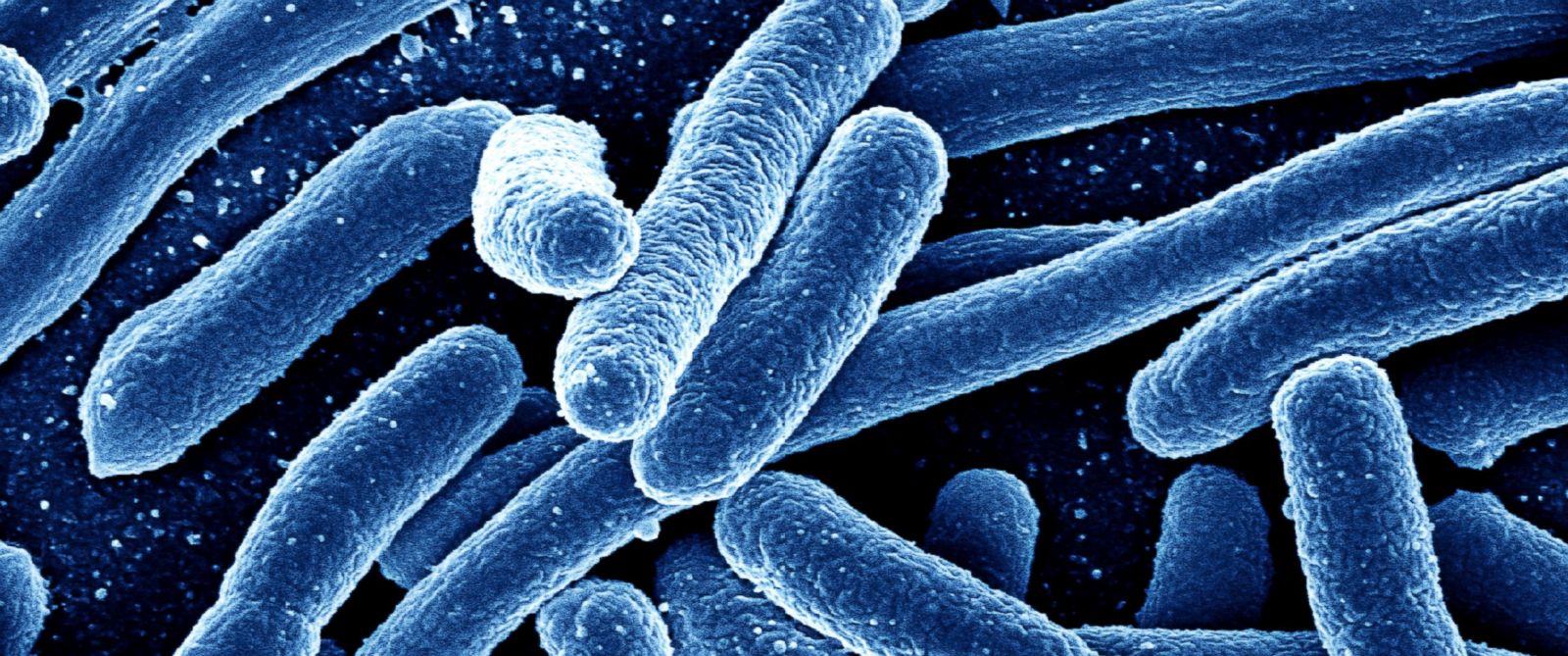
Since Alexander Fleming came across penicillin in 1928, it and other antibiotics have saved many lives from diseases such as cholera, meningitis, and tuberculosis. However, their effectiveness led many health professionals to overprescribe antibiotics without checking if the treatment would affect the microorganism causing the disease.
Antibiotics did not discriminate against their targets. They would take out any microbe that they came across, including the good bacteria that live inside the gut.
The human gut microbiome could not recover on its own from the devastating effects of antibiotics. It needed the help of its host, who needed to increase his or her intake of healthy bacteria.
Most health professionals would not be able to provide their patients with the right advice on restoring the population of good bacteria in the gut. Their training didn't cover how to rebuild the natural bacterial ecosystem inside the body. (Related: Candida Auris: The silent superbug that’s already too late to stop – full documentary.)
Antibiotic overuse created superbugs that could withstand antibacterials
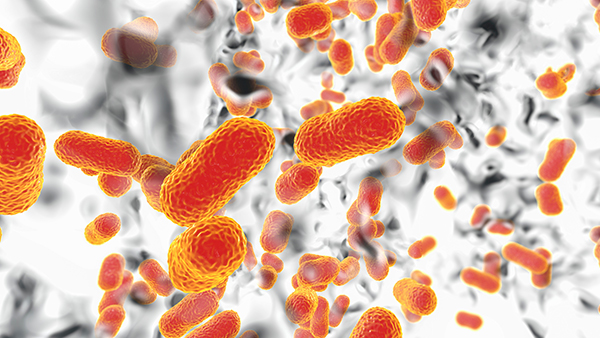
In addition to harming good bacteria, antibiotics also triggered the appearance of harmful bacteria that adapted themselves to resist the effects of antibacterials. Even increasing the dosage of existing antibiotics or creating new treatments failed to make headway against these mutated "superbugs."
The increasing number of antibiotic-resistant bacterial strains have forced health professionals to prescribe last line antibiotics more often. Those drugs were supposed to be last-resort treatments to prevent bacteria from developing a resistance to them. But they were now being used to try to stem the tide of drug-resistant diseases, at least until they stop being effective as well.
In the United States alone, more than two million cases of antibiotic-resistant diseases are reported every year. More than two percent of those patients would die from their infections. Around the world, the total death toll is now 700,000 -- and climbing.
Due to the spread of superbugs, public health authorities have expressed concerns about a "post-antibiotic world." By 2050, drug-resistant versions of bacterial diseases like pneumonia and urinary tract infections could kill millions of people every year.
Most antibiotics are used in factory farms run by the livestock industry
The overprescription of pharmaceutical antibiotics has contributed to the appearance of superbugs. But the biggest culprit of antibiotic overuse turns out to be the livestock industry.
To provide enough animal products for growing human populations, they came up with the concept of factory farming, where they raised vast numbers of broiler chickens and other livestock in enclosed areas. The combination of overpopulation, cramped spaces and unsanitary conditions made factory farms the perfect breeding grounds for bacteria.
The livestock industry abused antibiotics in two ways. First, they administered low doses of antibiotic drugs to all of the animals to prevent epidemics from breaking out and wiping out all of their livestock. Second, they did so to encourage the animals to put on weight very quickly.
The overuse of antibiotics in factory farms ensured the mutation of surviving bacteria into drug-resistant strains. These antibiotic-resistant microbes contaminated meat products, accounting for the 55 million cases of salmonella, listeria, and other food-borne diseases reported every year.
The best way to avoid these antibiotic-resistant superbugs is to adopt a plant-based diet. Be thorough in washing and cooking the raw foods. Any desired animal product should be obtained from organic farms that naturally raised their animals on pastures without using antibiotics.
Read more news about Big Pharma's toxic drugs at BigPharmaNews.com.
Sources include:
Please contact us for more information.