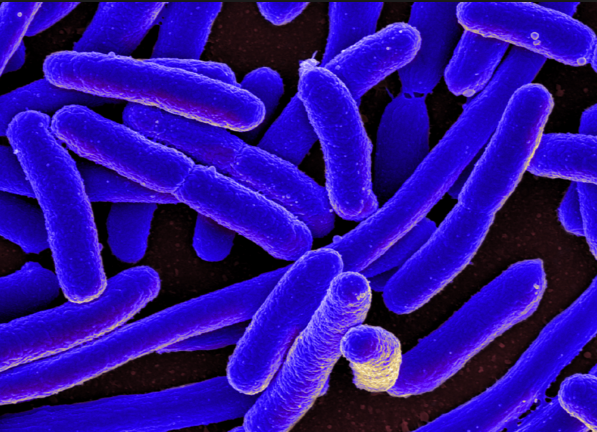
Staph, as the pathogen is more colloquially known, is a type of highly feared bacteria that can prompt the development of severe health conditions which can be fatal. When symptoms are at their height, a staph infection can cause bacteremia (sepsis in the bloodstream), pneumonia, endocarditis (infection of the heart valves), and osteomyelitis (bone infection). Antibiotics used to be effective at treating the infection; however, constant exposure to these drugs allowed the bacteria to mutate and develop a resistance. This caused alarm among medical health professionals who noted a significantly higher risk of a staph infection among those who had a compromised immune system. This included patients with chronic conditions such as diabetes, cancer, eczema, and lung disease.
Worse, more aggressive strains of the bacteria were observed quite recently. These strains, called community-associated MRSA (CA-MRSA) triggered extremely adverse infections in the skin and tissue even among healthy people.
Authors of the new study are hopeful that their investigation can create easier ways to treat the infection by understanding how the bacteria works. Unlike antibiotics that directly “fight” the bacteria, this new study disrupts natural processes.
“It’s well known that CA-MRSA strongly increases the secretions of toxins, which plays a major role in the serious progression of skin infections,” noted Dr. Christopher Weidenmaier who led the research group. “We’ve now also been able to prove that the increase insertion of the sugar polymer into the cell envelope creates a change in the immune reaction in the case of skin infections.”
What Dr. Weidenmaier is referring to is the outer cell envelope of the bacteria, which was found to react violently to increasing amounts of long-chain sugar polymers. This reaction fed the aggressive bacteria so that they were able to infect the skin in animal models. This shows a remarkable ability of staph to adapt to its environment and harm even healthy skin.
While more research is necessary to prove the same effect in humans, this does imply that CA-MRSA can be stopped by deliberating preventing its modification process. In this, scientists develop anti-virulence strategies that address the pathogenic effect rather than the pathogen itself. It is believed that such a course of action will reduce the likelihood of bacteria strains developing resistances to other medical forms of treatment.
“This kind of therapeutic approach would give the human immune system the chance to combat the infection more efficiently itself,” concluded Dr. Weidenmaier. “Because the bacterial cell is not killed off or inhibited in its growth, it is subject to less evolutionary pressure.”
On CA-MRSA
There are five strains of MRSA, but the most recently identified is the CA-MRSA. It differentiates from the others in that it can occur in otherwise healthy people. It is estimated that around 20 to 30 percent of the general population (across Canada and the Northern parts of the continental U.S.) carry the Staph bacteria on their hands or nose without presenting any symptoms. CA-MRSA is spread through direct physical contact or by touching or being exposed to objects contaminated with infected bodily fluids.
For the most part, CA-MRSA is spread in hospitals and other healthcare facilities. Athletes, prisoners, and people living in crowded settings are also vulnerable to catching the disease.
For more news on Staph and other bacterial infections, visit Outbreak.news.
Sources include:
Please contact us for more information.